I am passionate that we change the conversation when an individual is diagnosed with dementia about what can be offered to treat their condition and what options are available for their care. There’s been no new treatment licenced in the UK for Alzheimer’s disease for 20 years and the failure rate for drug trials, since 2002 (when the last drug was licenced) is a staggering 99.6%! At last we’ve had some promising positive news and we eagerly await the CLARITY study data release, with two other trials set to share their findings this year, as reported by the Alzheimer’s Society.
This is possible only through commercial drug companies committed to finding disease modifying drugs for Alzheimer’s disease and researchers’ relentless pursuits to find better treatments and ways of caring. However, ultimately, we cannot make progress unless those with the condition and their families participate in research. I am always staggered and impressed by their willingness to volunteer and help us shape research; to receive an experimental treatment where there may be side effects, where there may not be benefit to themselves and where there are frequent visits to the research site to undergo reams of questionnaires and clinical procedures.
At the UK Dementia Research Institute, Care Research & Technology Centre our aim is to enable people living with dementia to live at home, maintaining a good quality of life, for longer. We aim to do this via technology used in the home. We use both commercially available sensors (like movement sensors), or novel technology developed within the Centre. We have a cohort of people living with dementia (PLWD) and use artificial intelligence and machine learning to track movement (for example) to build a picture of individuals in the cohort. We aim to see where this typical behaviour deviates to try to predict when behaviour in the home changes and what this might mean for the PLWD and their families. We work this information into an algorithm and have a skilled team of research assistants who monitor the cohort and seek to validate these algorithms by providing support to build solid relationships with those taking part. This is to determine whether patterns we see generated from the sensors are related to any changes in behaviour in the home. One specific example of how we’re working to use this information is to see if we can predict when a PLWD has an infection and whether we can treat this, almost, before significant symptoms set in. We know that infections significantly increase a PLWD’s risk for developing delirium. If we can identify and treat infections in the earliest stages, it may be possible to prevent the PLWD developing delirium and therefore the need for a hospital admission.
The aim of this technology isn’t to replace human interaction and care, but rather to augment and assist clinicians by providing objective measures and insights into the data collected. To do this we are working with health and social care partners, charities, PLWD and their families to try to ensure the technology developed is fit for purpose, that privacy issues are fully discussed and disclosed, and that technology will be used by both PLWD and health providers alike.
We also see this technology being used to track and monitor both the progression of disease and the impact of medication. Once validated we hope to be able to use this technology within drug trials to add value to the existing pen and paper assessments to provide a holistic picture of how the participant is doing, to add to the body of evidence for drug efficacy (or non-efficacy!). There are many reasons why we’ve seen no new treatment for 20 years, and this blog post isn’t long enough to discuss even half of these reasons! However, the use of technology within these trials is currently limited and there is great opportunity to augment the data we are collecting. If we can add to the body of evidence with meaningful real-world data just think about what we can achieve!

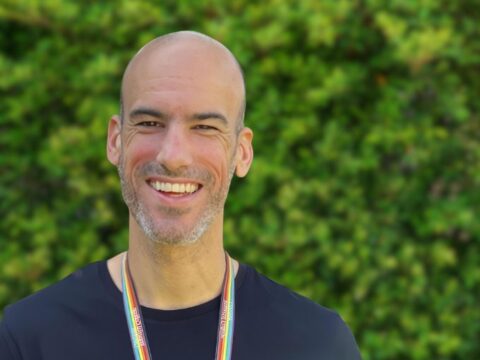
Danielle Wilson
Author
Danielle Wilson is a former acting director of a pre-eminent NHS centre conducting clinical trials & observational studies in across dementia & mental health conditions, and is the current Centre and Research Commercialisation lead at UK Dementia Research Institute, Care Research & Technology at Imperial College London. Danielle has extensive clinical research experience working with the National Institute of Health Research networks, the University of Oxford, the National Health Service (including Oxford University Hospitals NHS FT), Clinical Research Organisations & global pharmaceutical companies. She has experience working across medical specialities in a variety of human clinical trials, tissue, imaging & data studies. Passionate about patient care, participant safety & research excellence. Invested in staff development; most recently developed & implemented a competency framework for clinical researchers.
Danielle is also a Chair & long-standing expert member of a Health Research Authority research ethics committee leading a multidisciplinary group to review & give opinion on a broad range of studies, with particular specialism in applying knowledge of the mental capacity act to review research studies recruiting individuals who lack capacity.

 Print This Post
Print This Post