Over the last few months, I have often received the feedback that my blogs on maternity leave and parenthood are ‘open’ or ‘honest’. When invited to write these posts, my aim was to speak about anything that seemed important – no holds barred. For a few months there has been a topic I’ve been threatening to write on but avoided. However, it would be remiss of me to talk about becoming a parent without even vaguely alluding to birth.
Last month, as something of a throwaway comment, I mentioned the tendency in some circles to compare war wounds in relation to childbirth. After submitting the blog, I had a bit of a panic, worrying that this came across as needlessly glib, reducing what can be an incredibly traumatic experience for many women to a joke. Indeed, here in the UK, a report was published recently detailing the extent to which women suffer real and lasting trauma or injury as a result of inadequate maternity care. Now, I wouldn’t say that I had a particularly traumatic birth at all – but then, as a first timer, I didn’t really have a frame of reference. Apparently, I did.
Last summer, I listened to a podcast. The Retrievals told the story of a nurse who stole Fentanyl from the IVF clinic in which she worked, refilling the vials with saline. Moreso, it told the story of the women who were administered this saline, rather than the Fentanyl, while undergoing egg extractions. Instead of an incredibly powerful opioid, dozens of women went through an excruciating procedure with no pain relief. The women reported unbearable pain, would shake, cry out, scream. But they would not be believed. They were women; they were hysterical. This podcast stayed with me.
In October, with my due date approaching, a friend gave me some advice: when I think it is time to go to hospital, go to hospital. The hospital will tell me not to go, but I should go. A couple of weeks later, strangely, my midwife said the same thing. She commented that because I come across as pretty chilled out, the hospital would likely not believe I needed to go in, and that I should be firm and insist that I had to. I was confused – why would the hospital not believe me?
Fast forward to November, and two days before my due date, my contractions started. I was on a walk with my husband and casually mentioned that I had been experiencing some intermittent back pain. I was fine, it wasn’t really even painful. The following day, things escalated a bit. I still wouldn’t say I was in a lot of pain, but it was happening every 3 to 4 minutes, so calling the hospital seemed sensible. I explained the situation as clearly as I could, they thanked me for calling and told me I wasn’t in labour; I was a ‘first-time-mum’, and so it was no surprise I was panicking. I should have a bath. I didn’t really feel panicked.
Three hours later, at 1am on my due date, the contractions were well under 3 minutes apart and starting to be pretty painful, so I called again. I was clear, I was firm. I was told that I wasn’t in enough pain. If I was in labour, I wouldn’t be able to speak. Fair enough, I haven’t done it before. By 4am, the contractions were less than 2 minutes apart, and I was in so much pain that I couldn’t really imagine it being worse. For some reason, I remembered the podcast and the question that it posed: when it comes to reporting pain, can a woman be believed? If not, perhaps a man can? I asked my husband to phone the hospital. They still didn’t think I was in labour. But we’d called three times in 24 hours, so policy meant we had to be invited in. They stressed that if we arrived too soon, we would likely be sent home, so we should take our time. That was fine; it took 45 minutes for our friend to arrive to give us a lift, and another 45 minutes for me to get down the stairs, so by the time we got to hospital two hours had passed.
True to form, when I arrived, I was told that I clearly wasn’t in labour, but if I wanted they could do a quick exam to check on dilation. Sure, why not. Suffice it to say, this yielded different results to the cursory glance at my outward appearance, and my son was born within the hour. Turns out some people can walk or talk when in labour. Perhaps I’d been so focused on not coming across as hysterical that I’d gone too far the other way. But they’d accused me of panicking… what is this impossible balance?
It was fine, we were both relatively unscathed. Relatively. We were admitted to hospital for a week. On a couple of occasions, I was asked whether I was in pain. No, I said, I wouldn’t say I’m in pain. More… discomfort. In that, I feel too uncomfortable to walk, or sit, and need help to stand. But no pain – so no painkillers. Yes, I’d gone too far the other way. It was only on day 5 that a midwife insisted I be given painkillers, and asked whether she could make a couple of referrals for me, on account of the traumatic delivery. Traumatic? I hadn’t really noticed.
In the weeks and months that followed, my researcher brain kicked in. On a recent study, we used a quality-of-life outcome measure called the EQ5D-5L. One of the questions it asks is whether the person is in pain or discomfort. Could the nurses or midwives perhaps have asked me that instead? Would that have helped? A fellow conversation analyst PhD student visited me and the new baby. We talked about analysing phone calls between expectant mothers and hospitals, discovering the magic word that would lead to admission, comparing patient outcomes. It became something of a fixation.
I’m not sure of the purpose of this post. Maybe to publicly vent some of my private angst, although on the whole I don’t think I’m that self-indulgent. Perhaps to add fuel to the dumpster fire of medical misogyny. More than those, though, it’s likely part of my incessant need to illustrate the additional burdens that women carry when one might otherwise suppose they’re having a lovely break on maternity leave. Two weeks from the end of mine, I’m pleased to say birth is no longer dominating my thoughts, but that won’t be the case for all. Thankfully, I can focus on the baby, not the birth.

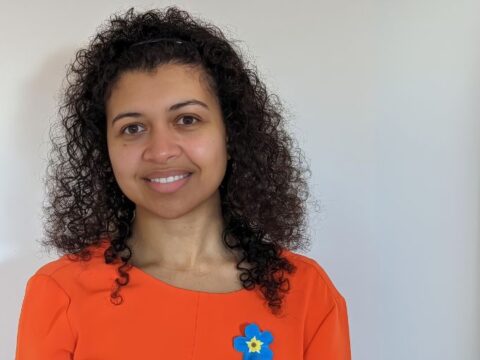
Emily Spencer
Author
Emily Spencer is a PhD Student at University College London looking at improving how GPs communicate with people with dementia and their family carers about their future care. Emily previous had a 5 year career break to pursue a career as a musician, and has previously undertaken research on improving the care people with dementia receive from their GP practice, as well as end-of-life and palliative care provision in the community. Emily is also a new mum and will be writing about her experiences navigating motherhood and a research career.

 Print This Post
Print This Post