I can do nothing but apologise for those of you sick of hearing my opinions on women in science, the state of academia and the best ways to write things. So for your sake, today we will be talking science. Specifically, we will be talking about the blood brain barrier.
Let’s start with Paul Ehrlich in the late 1800s and some notes on why we should stop talking about Paul Ehrlich and the blood brain barrier. Ehrlich was trying to figure out how much oxygen was consumed by various organs in various organisms. His 1885 treatise entitled “Oxygen Requirements of the Organism: A Colour-Analytical Study” spends a depressingly long time talking about the properties of dyes and oxidation-reduction reactions before heading into the experimental methods and results. Which is also long, detailed and very painful to read. He was using a dye called alizarin blue, which is extremely blue (for want of a better phrase) in areas of high oxygen consumption. Ehrlich injected rabbits with alizarin blue, not mice as is often quoted, and studied their organs. Interestingly he found that “the central nervous system gives a very distinct picture, in that the white substance is completely free of dye, while the grey has absorbed it in abundance and thus stands out most sharply in all its contours”.
Which, as you budding chemists in the audience have already spotted, is not really a description of the blood brain barrier but rather a description of the metabolic characteristics of grey and white matter. The actual first description of the blood brain barrier didn’t arrive until about 15 years later, in Max Lewandowksy’s paper where he was investigating the penetration of potassium ferrocyanide into various tissues. He noted that there was something preventing the passive diffusion from the blood to the brain as well as from the blood to the cerebrospinal fluid. This came off the back of some work by Biedl and Kraus in 1898, who were studying the behavioural effects of various bile salts (please don’t ask why) and found that there often weren’t any. They also theorised that this was because there was something which prevented solutions from just passing from the blood into the brain.
Interestingly, the first use of the term ‘barrier’ to refer to this phenomenon is thought to be by Stern in 1918. Ehrlich, by this time, was firmly of the opinion it was all a hoax. He said that he felt “unable to accept that the vascular endothelium, as such, exercises different functions in different organs”. So what is it about the vascular endothelium in the brain which is different from the vasculature elsewhere?
We’ll begin with the endothelial cells. These are the mainstay of the vasculature and in the blood brain barrier they are connected by tight junctions. There are tight junctions elsewhere in the vascular tree, usually in larger vessels with high flow rates, but in the brain the tight junctions go all the way down to capillaries and post-capillary venules. These tight junctions are formed by a network of proteins which basically bind the endothelial cells tightly together and prevent the random passing of most things into your brain.
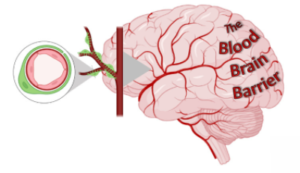
The blood-brain barrier (BBB) is the specialised system of brain microvascular endothelial cells (BMVEC) that shields the brain from toxic substances in the blood, supplies brain tissues with nutrients, and filters harmful compounds from the brain back to the bloodstream.
The endothelial cell tight junctions in the brain are induced and maintained by two of our other major cell types. Astrocytes and pericytes. Astrocytes are star-shaped cells which play a major supporting role in the brain. Like the brains lab managers they do everything from mopping up excess neurotransmitter to projecting end-feet to support barrier development. And next to them at the barrier are pericytes. Anyone in the know, knows that pericytes in the brain are a contentious subject which is way too big for this blog but feel free to go and do some solo reading. Basically these cells wrap themselves around capillaries and post-capillary venules to support the blood brain barrier. They play a role in regulating blood flow as well as provide some basic immune functions.
Together the role of all of these cells is to keep the majority of stuff from getting into your brain. Things that float around in your circulation all the time that you really don’t want in there like angry immune cells. So under normal circumstances your blood brain barrier functions as a bouncer to your brain, regulating what gets in and what doesn’t.
But during trauma and disease things can, and do, go horribly wrong.
In stroke, there is no opening in the very first minutes after the clot arrives but within hours the blood brain barrier becomes dysregulated. The release of superoxide and other free radicals begin to affect the junctional proteins so the tight junctions between the cells become loose. Enzymes such as the metalloproteinase family begin to break down these protein complexes, making the barrier leaky. Astrocytes withdraw their end-feet. Pericytes constrict and die. And these effects have been shown to last for several weeks in people, depending on the type and location of the stroke. This allows all sorts of floating circulating immune cells, like neutrophils, to get into your brain and wreak all kinds of havoc.
In dementia, the role of blood brain barrier dysfunction is less clear. Studies have shown that the pericytes, some of the supporting cells wrapping around capillaries, are amongst the first cells to fail in Alzheimer’s. This causes a broad low-level leakiness of the barrier which often occurs prior to cognitive decline. There seems to be little to no association of amyloid and tau accumulation with blood brain barrier permeability, suggesting that these proteins, or toxic versions thereof, may not be playing a role in its demise. So, is the blood brain barrier permeability seen in dementia causative? Or does it happen as a result of the ongoing pathology, perpetuating the decline.
Beyond brain diseases, systemic issues such as hypertension can also affect the blood brain barrier. In a previous post on blood flow in the brain I described how high blood pressure can cause vascular remodelling and changes in endothelial cell function. Recent work has demonstrated that all the cells of the blood brain barrier are likely to be involved in the sensing of, and response to, hypertension. For example, astrocytes have been found to become more reactive under hypertensive conditions, producing neurotoxic substances such as free fatty acids. It’s known that patients with hypertension often do worse after traumas such as stroke, likely because their blood brain barrier is already failing.
So, what does this all mean for treatment of brain disease? Well, here is where it becomes a bit complex. In stroke and traumatic brain injury you might want to close the blood brain barrier to stop miscellaneous cells from getting in. But you might also want to keep it a little open to allow neuroregenerative therapies to pass through. In dementia you might want to open it further to allow for the efflux of tau and amyloid, or to allow therapeutic antibodies to get in. But you might also want to monitor it before cognitive decline and try and keep it closed to prevent onset.
Understanding the temporal dynamics of changes in the blood brain barrier are key to targeting it effectively. Finding out when, where and how the opening and closing of the barrier are causing neuronal death are going to be vital questions in the development of novel therapies. But studying endothelial cells, or pericytes, or astrocytes, or even microglia and neurons, in isolation won’t give us a full picture. We need to think about the interactions between these cells at different stages of disease, and in response to therapy, in order to really appreciate and conquer the blood brain barrier.

Dr Yvonne Couch
Author
Dr Yvonne Couch is an Alzheimer’s Research UK Fellow at the University of Oxford. Yvonne studies the role of extracellular vesicles and their role in changing the function of the vasculature after stroke, aiming to discover why the prevalence of dementia after stroke is three times higher than the average. It is her passion for problem solving and love of science that drives her, in advancing our knowledge of disease. Yvonne has joined the team of staff bloggers at Dementia Researcher, and will be writing about her work and life as she takes a new road into independent research.

 Print This Post
Print This Post